Letter from London: The NHS in the UK 2020. What does it mean to people?
By Anthony Goodman and Sue Goodman

Margaret Thatcher famously said that there was no such thing as society. The current coronavirus and the magnificent recent response of the majority of people in the UK demonstrates that this very selfish and narrow view of society is very wrong. Indeed, on 30 March 2020 the current Prime Minister, recovering from the coronavirus, commented that “One thing the coronavirus has proved is that there really is such a thing as society.” How times change!
The NHS is an important icon for all that is best in British society and no political party would dare to try to end it. Having said that, in recent years under different conservative governments, there has been a move towards hiving off elements into the private sector. Perhaps now this will be rolled back or will not continue. With the ending of European Union membership and moves to move closer to other countries, including the United States, there has been discussion whether this would open up the NHS to competition, whether it is ‘up for sale’? This, and the importing of chlorinated washed chicken, would generate much media attention.
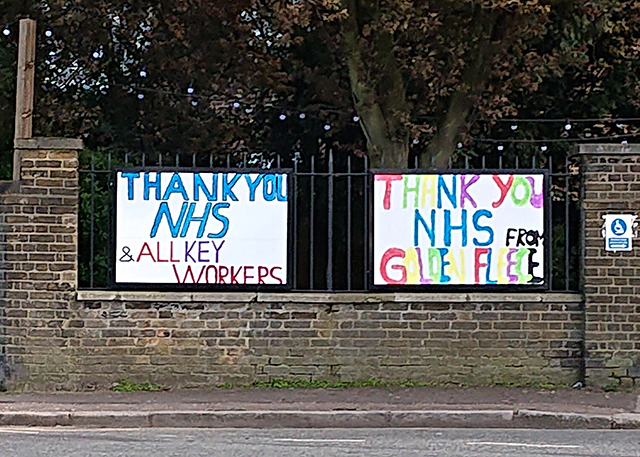
At 8 pm on 26 March 2020 after a tweet went viral, many members of the British public went to their front doors and windows, or to their balconies, with saucepans and spoons, or just their hands, to applaud the work being carried out by NHS staff throughout the UK. The response to a government request for recently retired and newly qualified staff to join the NHS has also been remarkable.
Both of Sue’s parents were doctors, and she can recall her mother telling her of her joy at the foundation of the NHS on 5th July 1948, less than a month before she was born. Healthcare for everyone, taking away, for example, the need for parents to choose which prescribed medication they could afford to buy for their sick children.
Every day, during the COVID 19 pandemic, there has been public praise for the work of all healthcare staff. There has been severe disruption of normal operations. Regular outpatient appointments have been cancelled, although for some, phone consultations have replaced them. Routine operations have been postponed. Concentration is being put into supporting people who are seriously ill. Anthony’s brother, recently diagnosed with non-hodgkin lymphoma has started chemotherapy, a sudden temperature spike and emergency call for an ambulance resulted in instant hospital admission and treatment. The system is under serious pressure but is functioning.
It does appear that, much as it has been felt, before this emergency, the NHS was at breaking point, with successive governments continuing to encourage outsourcing and privatisation of services, the present situation has brought the nation together to provide as much support as possible for NHS staff.
In 2019 Sue had prolonged treatment for non-hodgkin lymphoma. We are unable to think of any shortcomings in the care and professional support she received, or in the technology employed in diagnosing and treating her. We have nothing but praise for the NHS, as we watched very busy staff, at all levels, politely, professionally and passionately supporting and caring for her. In any consultation, when members of her family were present, they were always included and consulted. Sue was treated with dignity and compassion, especially when she was severely ill, and her needs, both medical and personal were met at all times: x-rays, biopsies, CAT scans, PET scans, stem cell transplant etc. all were made without heed of cost. It is free at the point of delivery.
Some ten years ago Anthony experienced some mild symptoms of chest discomfort when running and immediately after a GP visit was offered an ECG, a stress ECG and very quickly an angiogram. Two hours later he was told that an artery was completely blocked and immediately he had a stent fitted. There were no questions of cost, or waiting, it was an emergency and treated as such. That is the NHS at its best and how it has operated in the UK.

We asked a GP for their experience of working in the NHS at this time and these are her comments
I am a salaried GP (so employed by a practice) in the NHS in a big UK city. I’ve been working as a GP for about 18 months. We are currently in unprecedented times with the COVID-19 outbreak and facing problems that none of the staff at my practice have known in our lifetime.
We are a large practice so are lucky that we haven’t been as affected as some by current issues with staffing levels. Currently, any staff member who is unwell with possible CV symptoms has to be off work and self-isolate at home for 1 week but any household member has to self-isolate at home with them for 2 weeks. Many of the staff at my practice have young children with the usual coughs and colds common in this age group at this time of year, so they are having to stay off work for 2 weeks even if they feel completely well. We are able to do some things from home e.g. telephone consultations and look at blood results etc. This week we have been informed that testing is now available for some NHS staff locally – I think first for A&E, intensive care workers and paramedics. We are told that these may be available for GPs next week.
I have been lucky enough to not yet get ill and I live alone so no chance of needing to self-isolate due to a household member, so have been able to attend work on all my usual days. We are doing as many consultations as possible on the phone or on video consultations. Sometimes we are triaging patients on the phone but still needing to bring them in for physical examination. We are currently advised to wear PPE if the patient has had any cough or fever but if not, we are just advised to see them in usual clothing and not take any unusual precautions (apart from the usual hand washing and just being generally careful). The concern at the moment is that many asymptomatic patients are walking around so we are maybe seeing these patients about other issues and not realising. Unfortunately, we are not currently able to wear PPE with ALL patients as there is a worry that supplies will run out.
Most patients have been extremely understanding about the current situation and so we haven’t been overwhelmed with calls as I think many patients are postponing routine queries and problems. This is a worry as well as ‘after COVID-19’ (whenever that may be) we are expecting then a huge influx of people needing consultations about routine issues. Many of these may not actually end up being routine as they may be things that need referring urgently for suspected cancer but patients were not aware of the seriousness of symptoms or did not realise that suspected cancer referrals are still being seen at the moment. Therefore we are worried that cancers diagnoses may be delayed.
Currently we are being informed that all routine outpatient appointments and operations are being delayed locally (indefinitely) so we are getting lots of patient contacting us who are in pain and not sure what to do – difficult as we can only do so much! Referrals for suspected cancer are all running as usual as far as I am aware.
We are having meetings at work every morning to update each other on any changes to guidelines and advice and support each other. We’re a close team. In a lot of ways I feel lucky to be able to still be going in to work and having some sense of normality and contact with colleagues! I’m expecting things to be all change this week as our hospitals become saturated and there is overspill into the community. We have many elderly housebound patients who we’d usually visit regularly and we’re not really seeing at the moment – I worry about them!
I’m always proud to be part of the NHS but even more so at the current time as everyone is coming together and showing the best of themselves and their devotion to helping others. In our surgery we have all had a bit of a ‘calm before the storm’ feeling for the last few weeks and I expected the storm to hit us in the next 1-2 weeks. Everyone is keen to do whatever we can to help at the moment.
This sums up the current state of play that has seen the best and worst of the human condition. Empty shelves in supermarkets due to panic buying but overwhelmingly, a sense of altruism that we need to be thinking of each other at this time. Medical staff have come out of retirement to support the NHS and the public will be prepared to pay for its continuation as a public service. There would be a puzzled response to the question why the richest nation on earth has so many people without public health cover? The NHS may be under resourced and stretched but it holds a special place in the UK amongst its population and this will not change.
…
Another article of interest:
An often overlooked region of India is a beacon to the world for taking on the Coronavirus – The Southern Indian state of Kerala has led the way in the fight against the coronavirus pandemic enacting key public health measures as well as economic and social measures to protect the population